Suffering from eczema? Take a deeper dive to understand this common, itchy skin condition & the top self-care practices to help soothe it
In this article, we’ll delve into the symptoms, causes, emotional impact and most importantly, some at-home self-care strategies to help manage your eczema symptoms effectively.
What is eczema?
Eczema is a common skin condition that affects many people worldwide. The National Eczema Society estimates one in five children and one in ten adults in the UK suffers with the condition. Eczema describes a group of conditions that make your skin dry, irritated, itchy, red and cracked, with atopic eczema being the most common type. It’s usually a chronic condition that can affect people long-term and often ranges in severity with flares that can be brought on by periods of everyday stress, illness or allergy.
It’s part of a group of conditions described as “atopic” which means sensitivity to allergens. It can run in families, and often develops alongside other conditions, such as asthma and hay fever.
Also known as atopic dermatitis, atopic eczema is characterised by itchy, inflamed and often dry rashes and patches on the skin.
Eczema can affect people of all ages but commonly occurs during childhood and is often something that can come and go throughout your lifetime. While atopic eczema can occur anywhere on the body, it typically appears on the creases of the joints of the elbows and knees, though eczema on the face, neck, around the eyes and eyelids and on the hands is also common.
What causes atopic eczema?
The cause of atopic eczema is complex and there are a number of factors that can lead to a person developing the condition. Typically, people with eczema have an increased inflammatory and allergy response in their skin cells and immune system. This means environmental triggers can cause flare ups in symptoms such as rashes and itching.
There is also a genetic link to the chances of developing atopic eczema, meaning that if a person has family members with atopic eczema, it is more likely that they can also go on to develop it. Atopic eczema also seems to run hand in hand with other atopic conditions such as hay-fever and asthma, meaning that people who suffer from one of both of those, may be more likely to have eczema also.
Some key factors that may cause the development of atopic eczema include:
Genetics: People with a family history of eczema, allergies or asthma are more likely to develop atopic eczema themselves. There is also evidence to suggest a link between atopic eczema and an alteration in a gene that is responsible for maintaining a healthy skin barrier. This allows moisture to escape and allergens to penetrate the skin, causing an inflammatory response and potentially triggering symptoms.
Allergens: Exposure to certain factors within your environment can exacerbate atopic eczema symptoms. These triggers may include allergens such as dust, pollen, pet dander and even woollen clothing, or irritants such as harsh soaps, detergents or chemicals applied to the skin. In certain cases, food allergies can also be linked to a flare up in eczema symptoms.
Being unwell: Certain bacteria and viruses can trigger a flare up in atopic eczema — even a common cold.
Everyday stress: Emotional stress can also play a role in atopic eczema flare-ups.
Skin dryness: If the skin becomes too dry in a person with atopic eczema, it can start to itch and crack, so it’s important to keep the skin well moisturised to help prevent this.
What does atopic eczema look like & what are the symptoms?
At its mildest, atopic eczema is dry, itchy and irritating but more severe cases can see sore, weeping and blistering skin. Eczema patches can appear on any area of the skin and often look bumpy and inflamed. Scratch marks in the area affected are common, as the person responds to the itching.
Key symptoms of atopic eczema include:
Itchiness: The main symptom of atopic eczema is intense itching. This itching can become so severe that it leads to scratching, which in turn inflames the condition and can lead to the skin becoming infected.
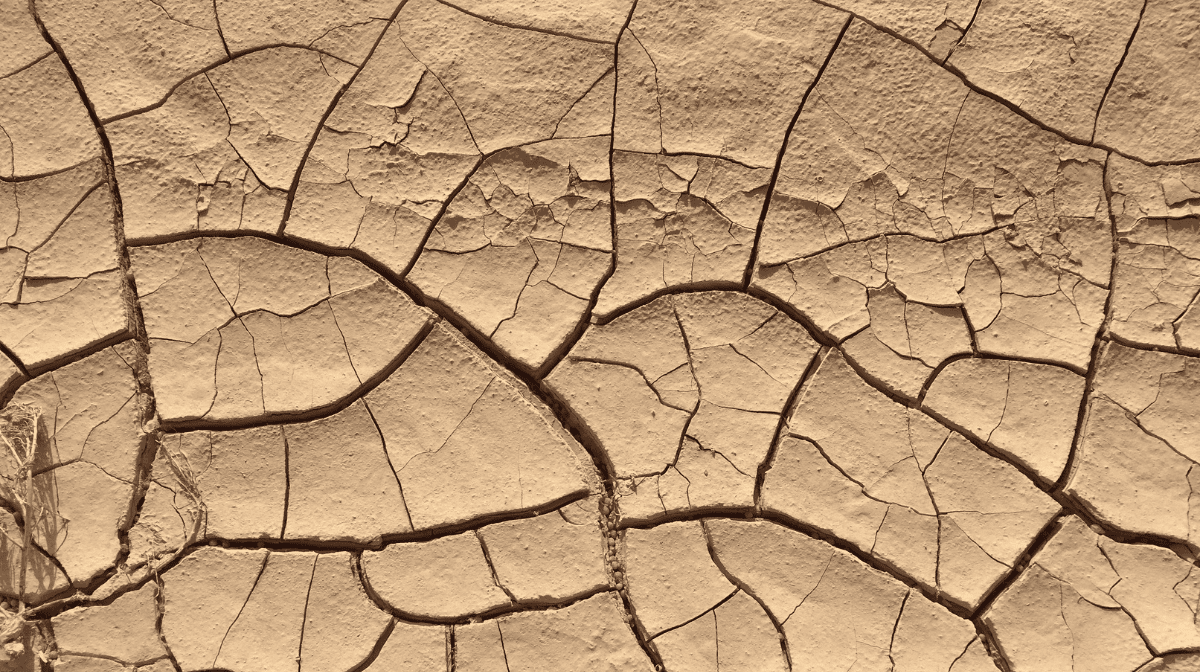
Dry, sensitive skin: People with atopic eczema often have dry and highly sensitive skin due to changes in the skin’s barrier not allowing it to retain enough moisture. The skin may appear flaky, rough or cracked.
Redness and inflammation: The word eczema comes from the Greek word “to boil” which refers to the redness and inflammation that is frequently seen in eczema-prone skin. This redness can be seen in smaller patches or spread over larger areas of the body.
Rashes and bumps: Atopic eczema can cause the development of rashes and small, raised bumps on the skin. The texture of the skin can become uneven or thickened due to inflammation and damage caused by scratching.
Weeping and blisters: In severe cases, atopic eczema may lead to very sore weeping, crusting or blistering of the skin, indicating a more acute flare-up.
Bleeding: Often the affected areas of skin become so itchy that a person scratches them, resulting in bleeding. This can also happen when skin gets excessively dry and cracks in the skin begin to split.
Is there an emotional impact of atopic eczema?
Suffering from atopic eczema can be tough physically and mentally for a person, however, with careful management, it shouldn’t stop you from living a full life and participating in activities such as sport, swimming and travel.
When someone is suffering from a flare-up in eczema symptoms, the itchiness can be severe enough to interfere with sleep, which in turn causes tiredness and irritability. This, combined with the impact of having physical changes to the appearance of their skin, can lead to a person experiencing a range of emotions, including embarrassment, self-consciousness, anxiety and frustration.
It’s understandable that atopic eczema can impact self-esteem and quality of life, sometimes leading to the person affected withdrawing from social and public situations. It’s essential to recognise the emotional and mental toll that eczema can take and seek support from your GP or mental healthcare professionals or support groups when needed. Seeking help for the emotional impact of eczema can be just as important as addressing the physical symptoms.
How can lifestyle & self-care changes help atopic eczema?
Alongside working with your healthcare professional on a treatment plan, there are several lifestyle and self-care strategies that may help alleviate symptoms:
Moisturiseregularly: Keeping the skin well hydrated is essential. Use fragrance-free, hypoallergenic moisturisers and creams for eczema to prevent dryness and itching. Bathing and washing with a moisturising emollient instead of soap or shower gel is also very important, and if under control, the daily use of a moisturiser and gentle cleanser.
Choose skin-friendly products: Opt for gentle skincare products which support the skin’s natural barrier. Avoid chemicals and fragrances which can irritate sensitive skin.
Avoid triggers: It can be helpful to keep a diary to track potential triggers such as foods, allergens, products and environmental factors. Once you have identified things that make your eczema worse, you can try to avoid or minimise exposure to these where possible.
Keep cool: Taking short, lukewarm baths with an emollient or cool showers can help soothe irritated skin. Overheating can trigger irritation on the skin.
Loose natural fibre clothing: Wear loose-fitting, breathable, and soft cotton or silk clothing to minimise skin irritation. Avoid wool and synthetic materials which may trigger itching.
Manage everyday stress: Practise stress-reduction techniques such as yoga, meditation or deep breathing exercises to minimise emotional triggers.
Keep nails trimmed: short, clean nails can reduce the risk of infection and skin damage during eczema flare-ups.
Laundry: Wash clothes with a non-biological washing powder and ensure laundry is rinsed well to remove detergent residues.
Is it necessary to seek medical advice?
If you suspect you have eczema or have already been diagnosed, seeking guidance from your GP is essential. They can provide a personalised treatment plan tailored to your unique condition and symptoms.
If you feel your eczema has become infected, it is strongly advised to seek immediate medical advice from your GP.